Lymphatic Filariasis - Social Issues | UPSC Learning
Topics
0 topics • 0 completed
🔍
No topics match your search
Lymphatic Filariasis
Medium⏱️ 12 min read
social issues
📖 Introduction
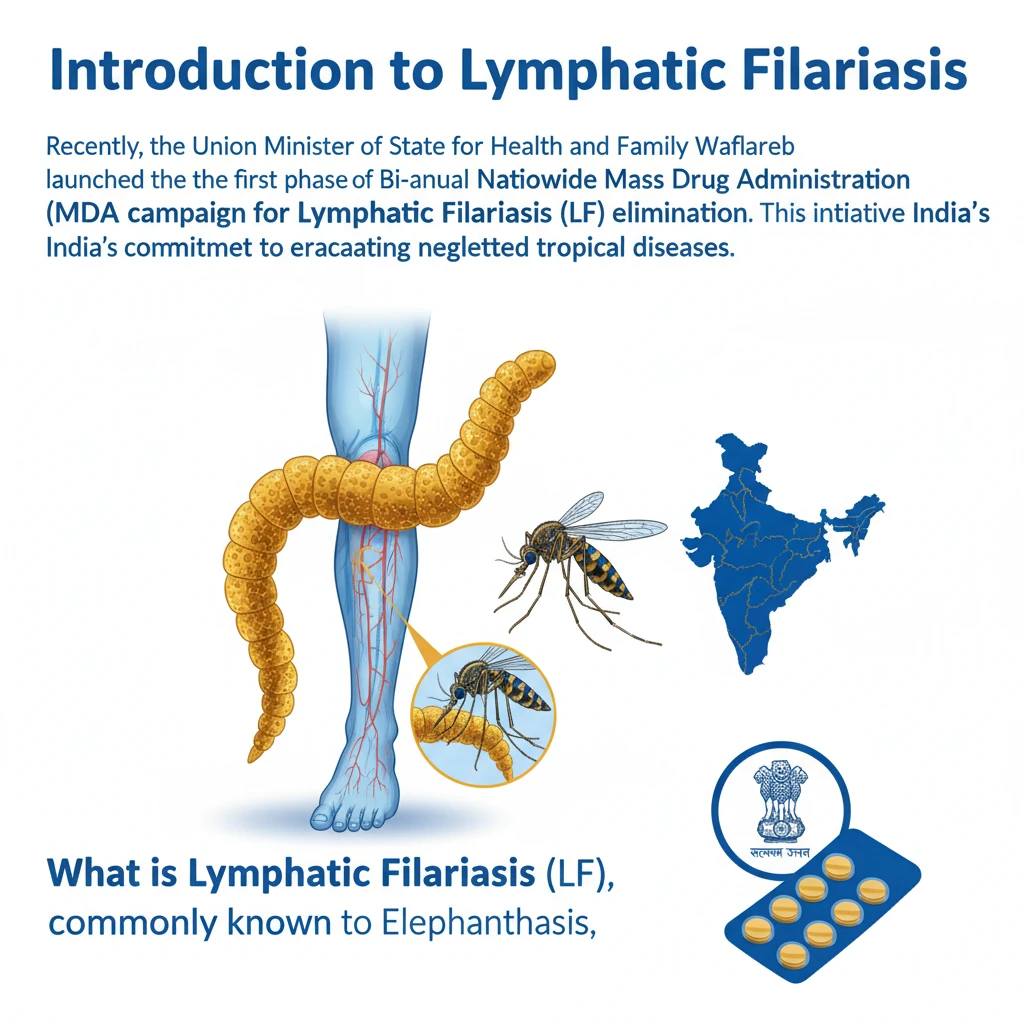
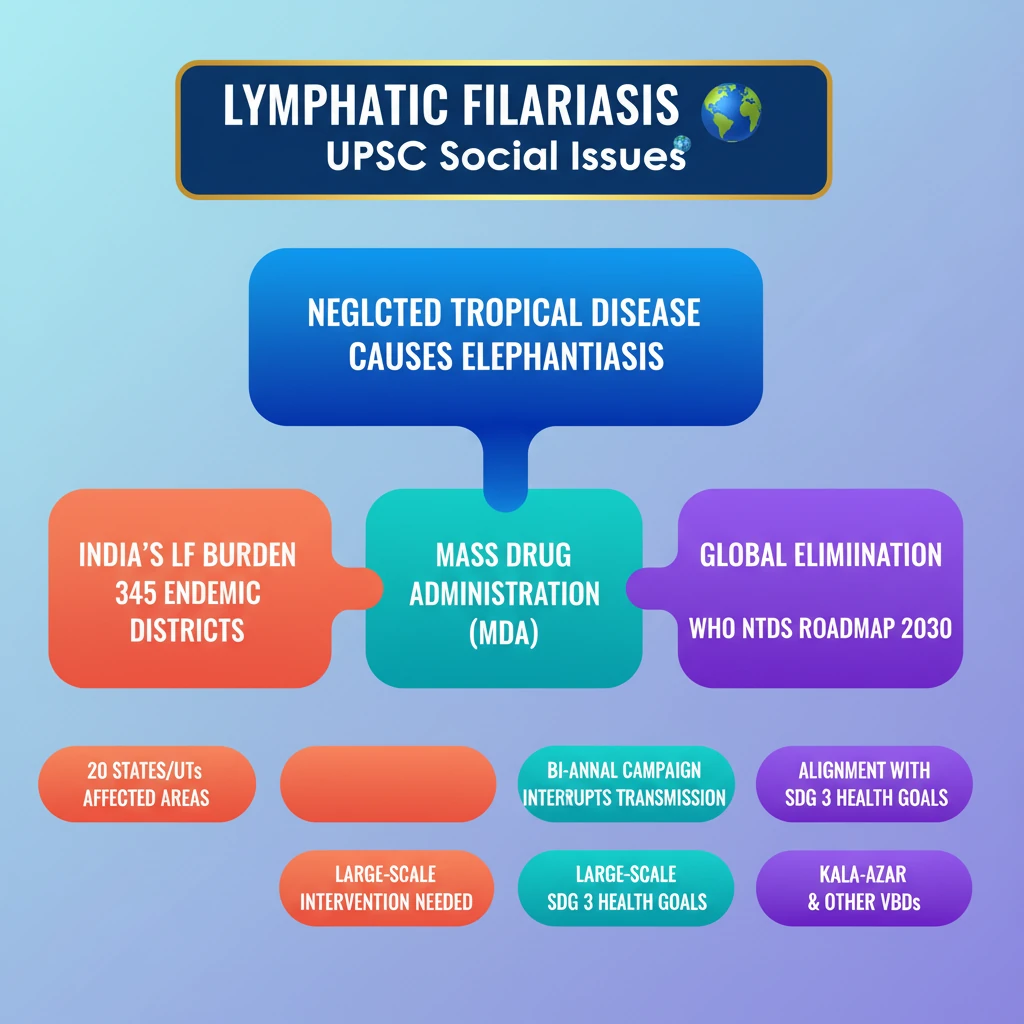
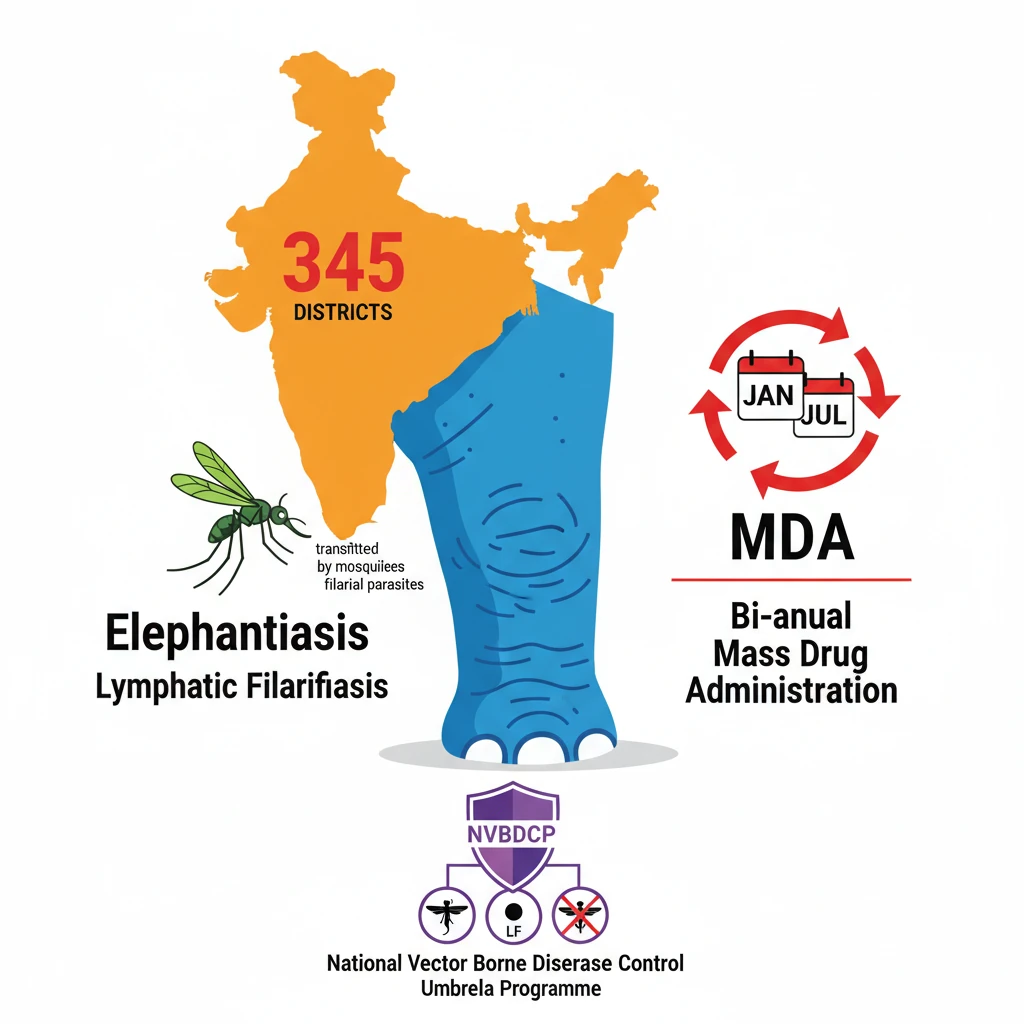
<h4>Introduction to Lymphatic Filariasis</h4><p>Recently, the <strong>Union Minister of State for Health and Family Welfare</strong> launched the first phase of the <strong>Bi-annual Nationwide Mass Drug Administration (MDA) campaign</strong> for <strong>Lymphatic Filariasis (LF) elimination</strong>. This initiative underscores India's commitment to eradicating neglected tropical diseases.</p><h4>What is Lymphatic Filariasis?</h4><p><strong>Lymphatic Filariasis (LF)</strong>, commonly known as <strong>elephantiasis</strong>, is a debilitating <strong>neglected tropical disease (NTD)</strong>. It is caused by infection with <strong>filarial parasites</strong> which are transmitted to humans through <strong>mosquito bites</strong>.</p><div class='info-box'><p><strong>Definition:</strong> Lymphatic Filariasis is a parasitic disease caused by thread-like worms that block the lymphatic system, leading to severe swelling and disfigurement, primarily in the limbs and genitals.</p></div><h4>Global and National Prevalence of LF</h4><p>In <strong>2021</strong>, approximately <strong>882.5 million people</strong> across <strong>44 countries</strong> lived in areas requiring preventive chemotherapy. This highlights the widespread global burden of Lymphatic Filariasis.</p><p>In India, LF remains a serious public health challenge. Currently, there are <strong>345 Lymphatic Filariasis endemic districts</strong> spread across <strong>20 states and union territories</strong>.</p><ul><li>Approximately <strong>75% of the Mass Drug Administration (MDA) districts</strong> are concentrated in five states: <strong>Bihar, Jharkhand, Uttar Pradesh, Odisha, and Telangana</strong>.</li><li>The disease is more prevalent among the <strong>urban poor</strong> but also significantly affects all segments of the <strong>rural population</strong>.</li></ul><h4>India's Recent Initiative: Mass Drug Administration (MDA) Campaign</h4><p>The recently launched <strong>Bi-annual Nationwide MDA campaign</strong> aims to interrupt disease transmission. It achieves this by providing free preventive medications to residents in affected areas.</p><div class='key-point-box'><p><strong>MDA Campaign Goal:</strong> To check disease transmission by administering preventive medications. The initial phase of the campaign is set to cover <strong>92 districts across 11 states</strong>.</p></div><h4>Related Neglected Tropical Disease: Kala-Azar</h4><p>While the primary topic is Lymphatic Filariasis, the source material also details aspects of <strong>Kala-Azar</strong>, another significant <strong>neglected tropical disease</strong> in India. Control efforts for various vector-borne diseases often share common strategies and programmatic frameworks.</p><h4>Diagnosis and Treatment of Kala-Azar</h4><p>Suspected cases of <strong>visceral leishmaniasis</strong>, commonly known as <strong>Kala-Azar</strong>, require immediate medical attention. Diagnosis involves assessing clinical signs combined with specific parasitological or serological tests.</p><div class='info-box'><p><strong>Mortality Rate:</strong> If left untreated, Kala-Azar can be fatal in <strong>95% of cases</strong>, underscoring the urgency of early intervention.</p></div><h4>Prevention and Control of Kala-Azar</h4><p>Effective prevention and control strategies are crucial for reducing the prevalence of Kala-Azar, preventing disabilities, and saving lives.</p><ul><li><strong>Early Diagnosis and Prompt Treatment:</strong> These are paramount in reducing disease burden and preventing severe outcomes.</li><li><strong>Vector Control:</strong> Measures such as <strong>insecticide spray</strong> and the use of <strong>insecticide-treated nets</strong> help reduce transmission by decreasing the population of <strong>sandflies</strong>, the disease vector.</li><li><strong>Effective Disease Surveillance:</strong> This is vital for monitoring disease trends, detecting epidemics early, and responding effectively to high case fatality rates.</li><li><strong>Social Mobilization and Partnerships:</strong> Community education and strong collaboration with various stakeholders are essential for successful control programs.</li></ul><h4>India’s Efforts to Control Kala-Azar</h4><p>The Government of India has a long-standing commitment to eliminating Kala-Azar through various programmatic interventions.</p><ol><li>The government launched a centrally sponsored <strong>Kala-azar control program</strong> in <strong>1990-91</strong>, which was subsequently revised in <strong>2015</strong>.</li><li>The program aimed to eliminate Kala-azar by <strong>2023</strong>, aligning with the <strong>WHO neglected tropical diseases (NTDs) Roadmap goal of 2030</strong>.</li></ol><div class='info-box'><p><strong>National Vector Borne Disease Control Programme (NVBDCP), 2003:</strong> This is an umbrella program that oversees the prevention and control of multiple vector-borne diseases, including <strong>malaria, lymphatic filariasis, kala-azar, and chikungunya</strong>.</p></div><h4>Recent Efforts Against Kala-Azar</h4><p>Recent initiatives have focused on multi-pronged strategies to combat Kala-Azar effectively.</p><ul><li><strong>Indoor Residual Spraying:</strong> Rigorous efforts are made to curtail <strong>sandfly breeding sites</strong> through indoor residual spraying. A special soil is also applied to seal crevices in mud walls, preventing sandflies from nesting.</li><li><strong>Housing Improvement:</strong> <strong>Pucca houses</strong> have been constructed in Kala-Azar affected villages under the <strong>Pradhan Mantri Awaas Yojana-Gramin (PMAY-G)</strong>. A total of <strong>25,955 houses</strong> were built in <strong>2017-18</strong> (11,371 in Bihar & 24,584 in Jharkhand).</li><li><strong>ASHA Network Mobilization:</strong> The <strong>Accredited Social Health Activist (ASHA) network</strong> is mobilized to ensure the completion of treatment for <strong>Post-Kala-Azar Dermal Leishmaniasis (PKDL) patients</strong>, who require a <strong>12-week course of Miltefosine</strong> (an antileishmanial agent).</li></ul><h4>Post-Kala-Azar Dermal Leishmaniasis (PKDL)</h4><p><strong>PKDL</strong> is a skin condition that can follow an episode of <strong>visceral leishmaniasis (Kala-Azar)</strong>. It manifests as rashes on the face, arms, and trunk.</p><div class='info-box'><p><strong>Prevalence:</strong> PKDL primarily affects regions like <strong>Sudan</strong> and the <strong>Indian subcontinent</strong>, with <strong>5-10%</strong> of Kala-Azar patients developing this condition.</p></div><p>PKDL may appear <strong>6 months to a year</strong> after the completion of Kala-Azar treatment. Importantly, individuals with PKDL can potentially serve as a reservoir, spreading <strong>Leishmania parasites</strong>.
💡 Key Takeaways
- •Lymphatic Filariasis (LF), or elephantiasis, is a neglected tropical disease caused by filarial parasites transmitted by mosquitoes.
- •India faces a significant LF burden, with 345 endemic districts across 20 states/UTs, necessitating large-scale interventions.
- •The Bi-annual Nationwide Mass Drug Administration (MDA) campaign is a key strategy to eliminate LF by interrupting transmission.
- •The National Vector Borne Disease Control Programme (NVBDCP) is an umbrella program managing LF, Kala-Azar, and other vector-borne diseases.
- •India's efforts to eliminate LF and Kala-Azar align with WHO's NTDs Roadmap 2030 and contribute to SDG 3.
- •Integrated approaches, including vector control, housing improvement (PMAY-G), and ASHA network mobilization, are crucial for effective disease control.
🧠 Memory Techniques
95% Verified Content
📚 Reference Sources
•World Health Organization (WHO) reports on Neglected Tropical Diseases (NTDs)
•Ministry of Health & Family Welfare, Government of India official releases