Post-kala-azar Dermal Leishmaniasis (PKDL) - Social Issues | UPSC Learning
Topics
0 topics • 0 completed
🔍
No topics match your search
Post-kala-azar Dermal Leishmaniasis (PKDL)
Medium⏱️ 7 min read
social issues
📖 Introduction
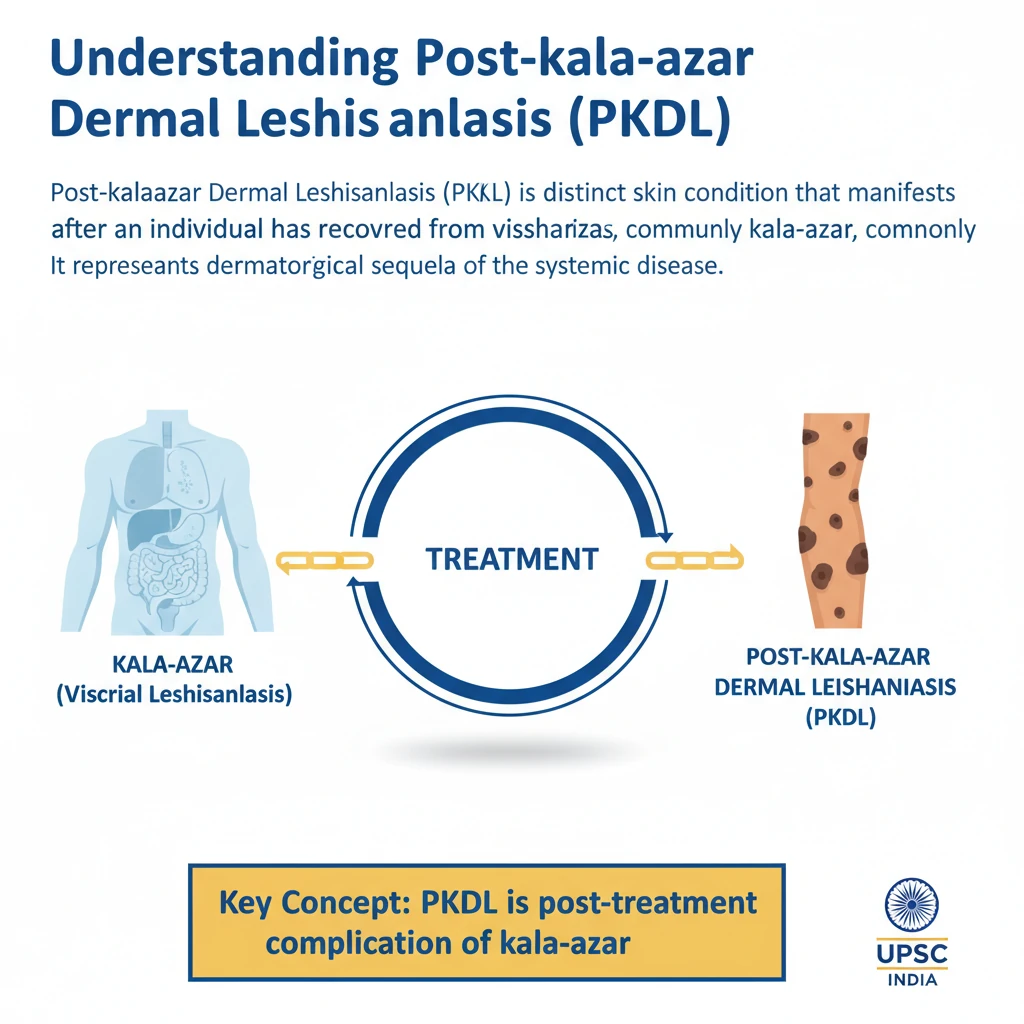
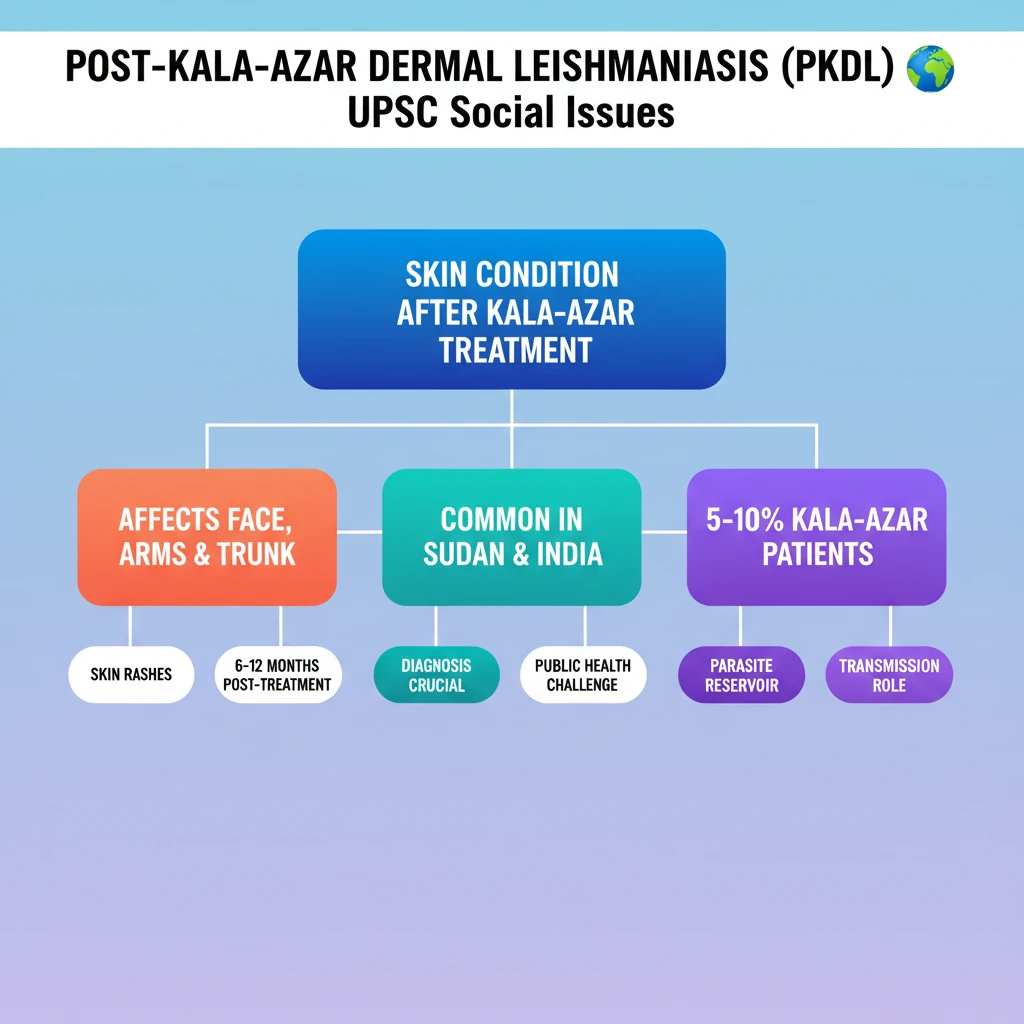
<h4>Understanding Post-kala-azar Dermal Leishmaniasis (PKDL)</h4><p><strong>Post-kala-azar Dermal Leishmaniasis (PKDL)</strong> is a distinct skin condition that manifests after an individual has recovered from <strong>visceral leishmaniasis</strong>, commonly known as <strong>kala-azar</strong>. It represents a dermatological sequela of the systemic disease.</p><div class='key-point-box'><p><strong>Key Concept:</strong> <strong>PKDL</strong> is a post-treatment complication of <strong>kala-azar</strong>, characterized by skin lesions.</p></div><h4>Clinical Manifestations and Symptoms</h4><p>The primary characteristic of <strong>PKDL</strong> is the appearance of various types of <strong>rashes</strong> on the skin. These lesions can present as macules, papules, nodules, or plaques, and their appearance can vary significantly among patients.</p><p>These distinctive rashes typically affect specific areas of the body. The most commonly involved regions include the <strong>face</strong>, the <strong>arms</strong>, and the <strong>trunk</strong> of the body. In some cases, lesions may also appear on other parts.</p><h4>Geographical Distribution and Prevalence</h4><p><strong>PKDL</strong> is not uniformly distributed globally. It predominantly affects certain geographical regions where <strong>kala-azar</strong> is endemic. The two major endemic areas are <strong>Sudan</strong> and the <strong>Indian subcontinent</strong>.</p><div class='info-box'><p><strong>Prevalence Data:</strong> Approximately <strong>5-10%</strong> of individuals who have previously suffered from <strong>kala-azar</strong> eventually develop <strong>PKDL</strong>. This indicates a significant proportion of treated patients are at risk.</p></div><h4>Timing of Onset and Transmission Risk</h4><p>The onset of <strong>PKDL</strong> is typically delayed following the successful treatment of <strong>kala-azar</strong>. It may emerge anywhere from <strong>6 months to a year</strong> after the completion of kala-azar therapy. This delayed manifestation makes surveillance crucial.</p><p>A critical aspect of <strong>PKDL</strong> is its potential role in the transmission cycle of <strong>Leishmania</strong> parasites. Individuals with active <strong>PKDL</strong> lesions can harbor the parasite in their skin, potentially acting as a reservoir for further spread of the disease by sandflies.</p><div class='exam-tip-box'><p><strong>UPSC Insight:</strong> Understanding <strong>PKDL</strong> is vital for comprehending the complete epidemiology of <strong>kala-azar</strong> and challenges in its elimination. Its role as a reservoir makes it a significant public health concern, often asked in <strong>GS Paper II (Health)</strong>.</p></div>
💡 Key Takeaways
- •PKDL is a skin condition occurring 6 months to a year after kala-azar treatment.
- •It primarily affects the face, arms, and trunk with rashes.
- •Prevalent in Sudan and the Indian subcontinent, affecting 5-10% of kala-azar patients.
- •PKDL patients can act as a reservoir, potentially spreading Leishmania parasites.
- •Crucial for kala-azar elimination efforts due to its role in sustained transmission.
🧠 Memory Techniques

95% Verified Content
📚 Reference Sources
•World Health Organization (WHO) reports on Leishmaniasis
•Indian Council of Medical Research (ICMR) publications