Leptospirosis Outbreak in Kerala - Science And Technology | UPSC Learning
Topics
0 topics • 0 completed
🔍
No topics match your search
Leptospirosis Outbreak in Kerala
Medium⏱️ 7 min read
science and technology
📖 Introduction
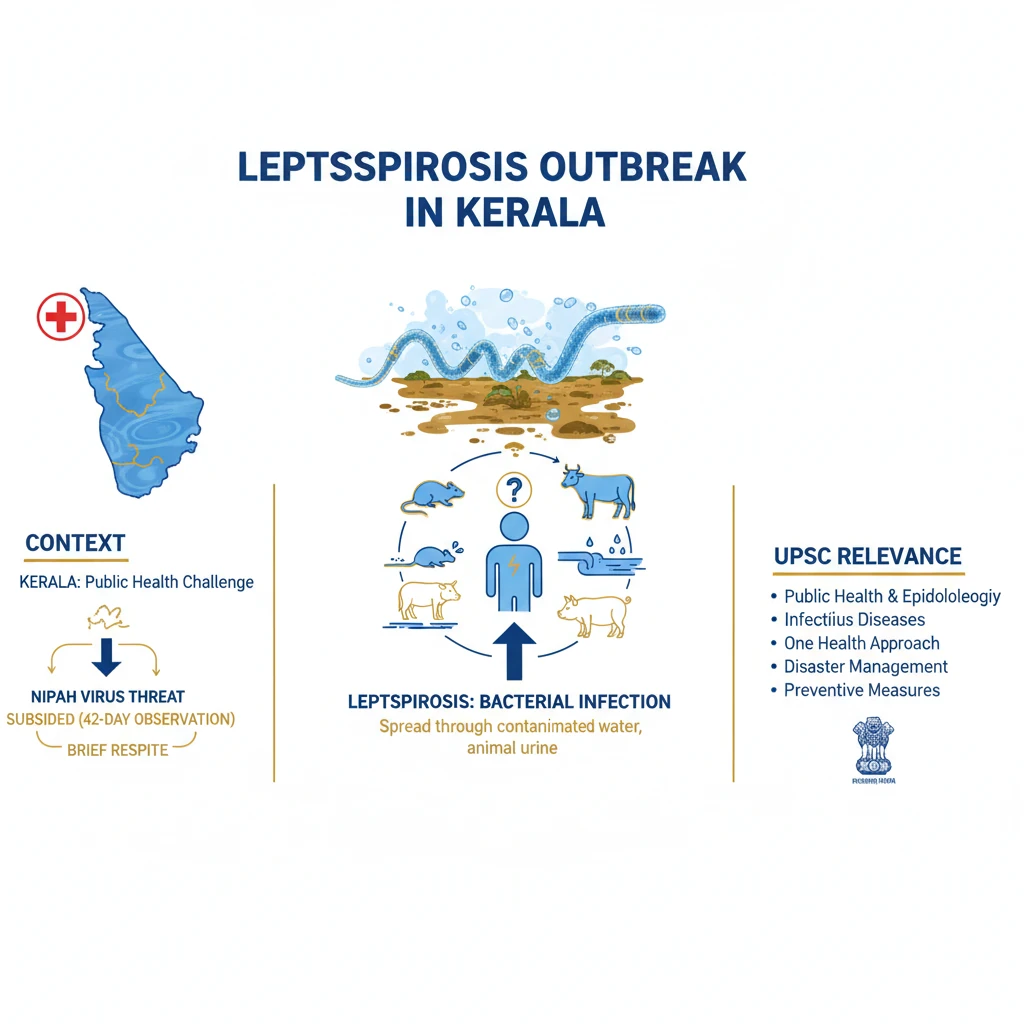
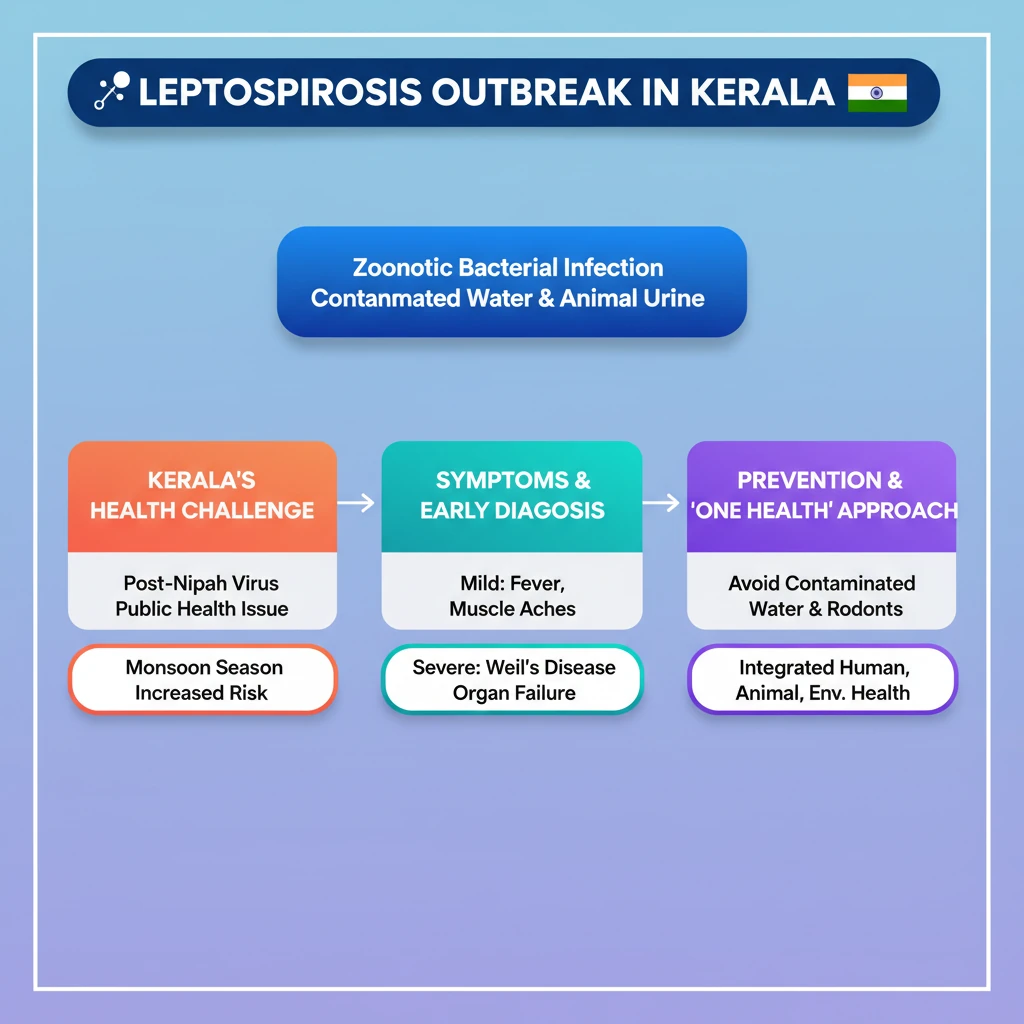
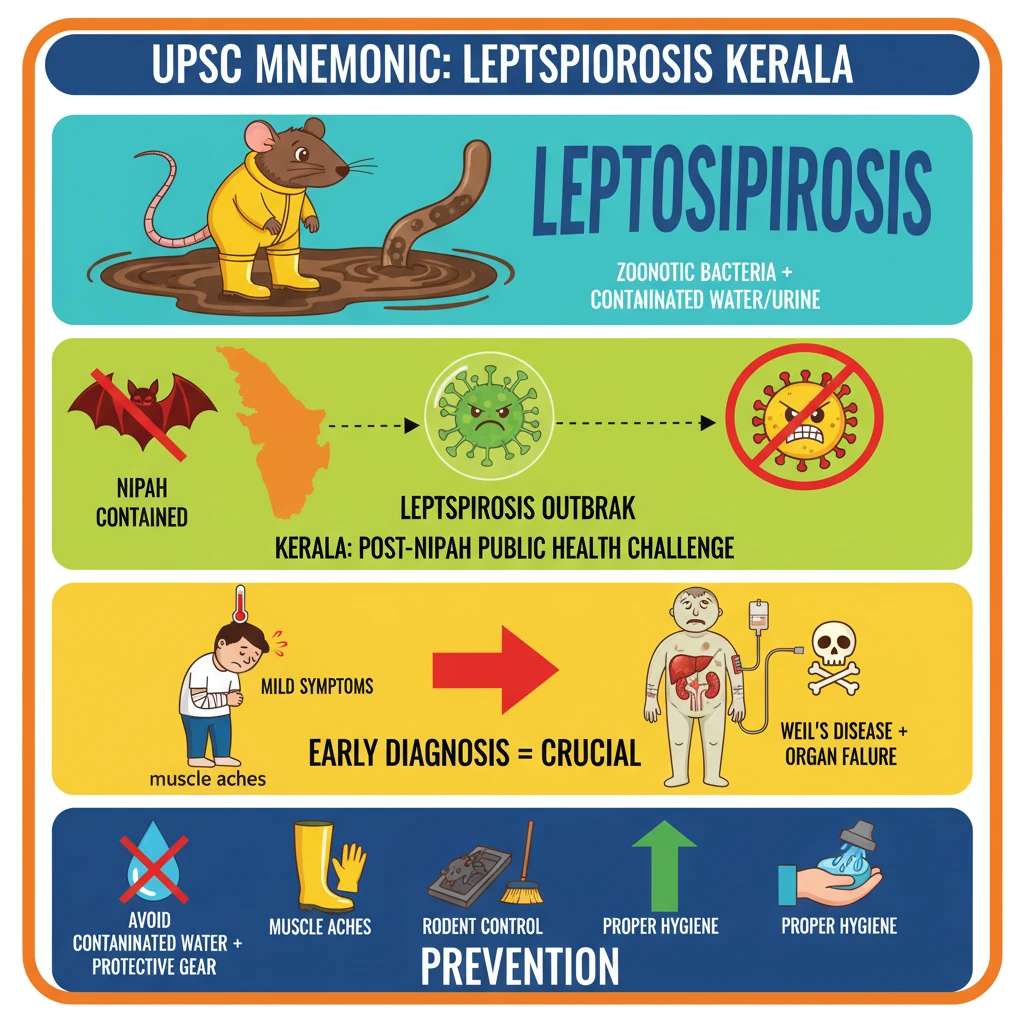
<h4>Context of the Outbreak in Kerala</h4><p>The state of <strong>Kerala</strong> recently faced a significant public health challenge with an outbreak of <strong>Leptospirosis</strong>. This emergence followed a period of relief, as the threat of a <strong>Nipah virus</strong> outbreak had subsided.</p><p>The <strong>Nipah virus</strong> situation was declared diminished after a crucial <strong>42-day observation period</strong> concluded with no new cases reported. This provided a brief respite before the new concerns regarding <strong>Leptospirosis</strong> surfaced.</p><div class='exam-tip-box'><p><strong>UPSC Insight:</strong> Understanding the sequence of public health events, like the transition from a <strong>Nipah threat</strong> to a <strong>Leptospirosis outbreak</strong>, highlights the dynamic nature of disease management and surveillance in states like <strong>Kerala</strong>, which are prone to such challenges.</p></div><h4>What is Leptospirosis?</h4><p><strong>Leptospirosis</strong> is a severe bacterial infection caused by bacteria of the genus <strong><em>Leptospira</em></strong>. It is a <strong>zoonotic disease</strong>, meaning it is primarily transmitted from animals to humans.</p><p>The bacteria are typically found in the urine of infected animals, including rodents, livestock, and pets. Humans can contract the infection through contact with contaminated water, soil, or animal urine.</p><div class='info-box'><p><strong>Key Fact:</strong> <strong>Leptospirosis</strong> is also known by various names such as <strong>Weil's disease</strong>, <strong>swineherd's disease</strong>, and <strong>rice field fever</strong>, reflecting its diverse sources and contexts.</p></div><h4>Transmission Pathways</h4><ul><li><strong>Direct Contact:</strong> Exposure to urine, blood, or tissues of infected animals.</li><li><strong>Indirect Contact:</strong> Contact with water or soil contaminated with infected animal urine. This often occurs during floods or heavy rainfall.</li><li><strong>Entry Points:</strong> The bacteria enter the body through cuts or abrasions in the skin, or through mucous membranes (eyes, nose, mouth).</li></ul><h4>Symptoms and Complications</h4><p>Symptoms of <strong>Leptospirosis</strong> can range from mild to severe and may appear 2 to 30 days after exposure. Initial symptoms often mimic other illnesses, making diagnosis challenging.</p><ul><li><strong>Mild Symptoms:</strong> Fever, headache, muscle aches (especially in calves and lower back), chills, red eyes, abdominal pain, diarrhea, and vomiting.</li><li><strong>Severe Symptoms (Weil's Disease):</strong> Can lead to severe forms affecting multiple organs, including kidney damage, liver failure (jaundice), meningitis, respiratory distress, and internal bleeding.</li></ul><div class='key-point-box'><p><strong>Important Concept:</strong> Early diagnosis and treatment are crucial to prevent severe complications and reduce mortality associated with <strong>Leptospirosis</strong>.</p></div><h4>Prevention and Control Measures</h4><p>Preventing <strong>Leptospirosis</strong> involves minimizing exposure to contaminated environments and infected animals. Public health strategies focus on awareness and hygiene.</p><ul><li><strong>Avoid Contaminated Water:</strong> Do not swim or wade in water that might be contaminated, especially after heavy rains or floods.</li><li><strong>Protective Gear:</strong> Use protective clothing, gloves, and footwear when working in areas with potential exposure (e.g., farmers, sanitation workers).</li><li><strong>Rodent Control:</strong> Implement effective rodent control measures in homes and communities.</li><li><strong>Animal Vaccination:</strong> Vaccinate pets and livestock where appropriate, and ensure proper disposal of animal waste.</li><li><strong>Hygiene:</strong> Wash hands thoroughly after contact with animals or potentially contaminated environments.</li></ul><h4>Treatment of Leptospirosis</h4><p><strong>Leptospirosis</strong> is treatable with antibiotics, which are most effective when administered early in the course of the disease. Common antibiotics include <strong>doxycycline</strong> or <strong>penicillin</strong>.</p><p>Severe cases may require hospitalization for intravenous antibiotics and supportive care, including management of kidney failure, respiratory distress, or other organ complications.</p>
💡 Key Takeaways
- •Leptospirosis is a zoonotic bacterial infection, often linked to contaminated water and animal urine.
- •Kerala's recent Leptospirosis outbreak followed the containment of a Nipah virus threat, highlighting ongoing public health challenges.
- •Symptoms range from mild (fever, muscle aches) to severe (Weil's disease, organ failure); early diagnosis is crucial.
- •Prevention involves avoiding contaminated water, protective gear, rodent control, and proper hygiene.
- •The 'One Health' approach is vital for managing zoonotic diseases, integrating human, animal, and environmental health strategies.
🧠 Memory Techniques
95% Verified Content
📚 Reference Sources
•World Health Organization (WHO) - Leptospirosis Fact Sheet
•Centers for Disease Control and Prevention (CDC) - Leptospirosis Information
•Ministry of Health & Family Welfare, Government of India - Public Health Guidelines
•National Centre for Disease Control (NCDC) - Annual Reports & Guidelines